
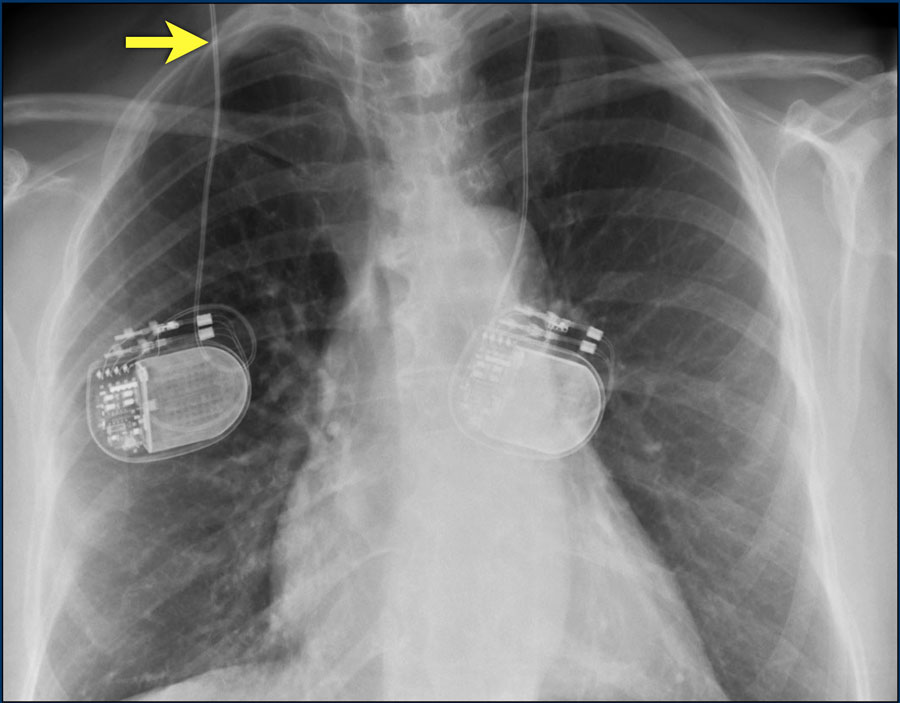
Sustained, fast, polymorphic ventricular tachycardia was easily induced, signifying that in addition to being at high risk for complete heart block and asystole, she was at significant risk for sudden cardiac death due to sustained malignant ventricular tachycardia. There was no evidence of a dual AV node physiology or an accessory pathway, but VA conduction was present. She was referred for a diagnostic EP study, which revealed a normal sinus node function, but a severely prolonged HV interval (104 ms). In view of these findings and the absence of an alternative diagnosis for her dizziness, she was considered at high risk for progression of cardiac conduction system abnormalities, given her history of DM. Pharmacologic single-photon emission computed tomography (SPECT) nuclear images with LEXI SCAN revealed no significant evidence for myocardial ischemia or transmural myocardial infarction. A 2-D echocardiogram showed a non-dilated left ventricle with mild, concentric, hypertrophy (LVH) and paradoxical septal wall motion abnormalities with an estimated left ventricular ejection fraction (LVEF) of 60%. There was an intraventricular conduction defect (IVCD) with a left bundle branch (LBBB) like morphology and QRS duration of 163 ms. The 12-lead EKG showed a rate of 69 beats per minute (bpm), first-degree AV block with a PR interval of 244 milliseconds (ms), and a left axis deviation. In this case series, we present nine cases of DM in a small, community-based teaching hospital that presented with various cardiac manifestations and received appropriate interventions, to prevent death from sudden cardiac arrest.Īn 82-year-old Caucasian woman with a medical history of hypertension and DM presented with episodes of recurrent lightheadedness, dizziness, and near syncope. Therefore, early electrophysiological (EP) studies are recommended to identify this subgroup and a prophylactic cardiac device (permanent pacemaker and ICD) placement is recommended for those at risk of severe bradycardia or malignant ventricular tachyarrhythmia.

However, recent studies have shown that ventricular tachyarrhythmias are possibly a more frequent cause of death than previously thought ( 5). Until recently, sudden death was thought to be primarily the result of conduction blocks.

The conduction abnormalities are seen in 65% of patients ( 5) and typically progress with gradual manifestation over many years however, the clinical course in an individual patient cannot be predicted.Ībout 20–30% of DM1 patients die due to cardiac causes ( 6–( 8)) of which one-third are from a sudden cardiac death. Cardiac manifestations are among the most common systemic features of DM and range from simple first-degree atrioventricular (AV) blocks to malignant ventricular arrhythmia. In general, DM is a multisystem disorder and typically presents as myotonia, muscle weakness, cataract, and cardiac conduction abnormalities ( 4). Based on the age at onset and symptoms, four clinical categories can be distinguished: congenital, childhood, classical (adult-onset), and mild (late-onset) ( 3). Type 2 (DM2) has an adult onset with a more favorable clinical course.ĭM1 results from an expansion of a repetitive trinucleotide segment in the 3′ untranslated region of the myotonic dystrophy protein kinase (DMPK) gene.

There are two distinct clinical forms, with type 1 (DM1) being more common with a prevalence rate of 1 in 20,000 ( 2). Even though the overall incidence is low, it remains the most frequently inherited neuromuscular disease of adult life ( 1).
Myotonic dystrophy (DM) is a group of inherited neuromuscular disorders with an autosomal dominant pattern of distribution.


 0 kommentar(er)
0 kommentar(er)
